Rectal Bleeding Facts
Rectal Bleeding Definition and Facts
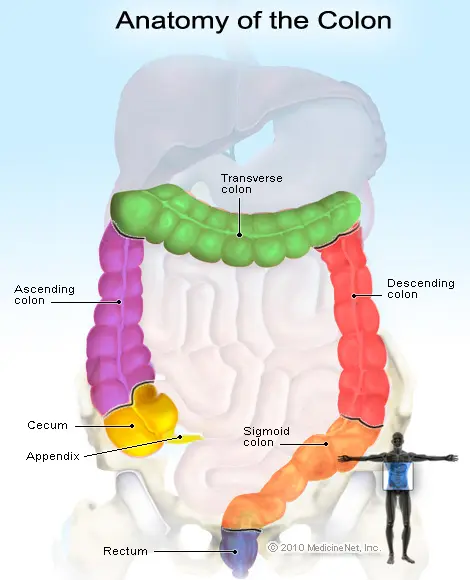
- The rectum is the last portion of the large bowel that ends just before the anus. Bleeding from this area can be mild, serious, or even life threatening; the presence of rectal bleeding must be carefully checked because it may indicate something is wrong somewhere else in the gastrointestinal (GI) tract.
- Seek medical care for rectal bleeding if accompanied by severe diarrhea, pencil-sized stools, nausea, vomiting, rectal trauma, irregular heartbeat, fainting spells, or difficulty breathing.
- Treatment of rectal bleeding depends upon the source and cause of the bleeding.
Causes of rectal bleeding are numerous and varied.
- Common anorectal causes are hemorrhoids, and anal fissures (tears in the rectal tissue),
- diverticula (diverticulitis, including Meckel's diverticulum),
- infections (bacterial and other pathogens),
- inflammatory bowel diseases (Crohn's disease and ulcerative colitis),
- angiodysplasia (fragile blood vessels),
- tumors,
- polyps, and
- bowel trauma.
- Less common causes include upper GI tract problems like ulcers and Mallory-Weiss tears in the esophagus or
- a dilated vein or varix.
Symptoms and signs of rectal bleeding frequently manifest as
- maroon-colored stools,
- bright red blood on or in the stool,
- blood on the toilet paper, or
- blood staining the toilet bowl water red.
Bleeding from further up in the digestive tract (stomach, small intestine, or large intestine) may result in black, tarry stools. Other symptoms associated with gastrointestinal bleeding include
- abdominal and /or rectal pain,
- dizziness,
- fainting,
- low blood pressure,
- vomiting,
- rapid heartbeat, and
- confusion.
Children may exhibit abdominal pains, vomiting and rectal bleeding; folding or telescoping of the bowel (intussusception) is a common cause.
Pregnant females often develop hemorrhoids during their second and third trimester. If a female has rectal bleeding during pregnancy she should contact her health care professional for evaluation of the cause.
When to Call the Doctor
Seek medical care to evaluate the source of bleeding; rectal bleeding with black or maroon-colored stools, large blood loss, rectal trauma, rapid or irregular heartbeat and/or fainting or confusion is a medical emergency. Call 9-1-1.
- Diagnosis of rectal bleeding depends on the cause; medical professionals diagnose some causes by the patient's history and physical exam while other causes require blood tests, scope exams of the bowel and/or CT scans, angiography or nuclear medicine studies.
- Treatment of rectal bleeding is dependent on the cause; simple treatments (some hemorrhoids, for example) can be done at home, but other more serious causes (tumors or ulcers, for example, may require much more effort like surgery and other therapy). Minimal rectal bleeding can be treated at home if the cause is known to be minor, but if it does not improve quickly or the person is 40 years of age or older, seek medical care.
- Follow-up is important in case the treatment is not effective or rectal bleeding starts again. The prognosis of rectal bleeding depends on the cause and the person's response to treatment. In general, those people who lose a small amount of blood do better than those who lose large amounts of blood (usually the elderly people with other medical problems).
What Is Rectal Bleeding (Hematochezia)?
Rectal bleeding (also called hematochezia, meaning bright red blood in the stool) is a symptom of a problem in the digestive tract.
- The definition is broad as it means any blood passed rectally; consequently, the blood may come from any area or structure in the GI tract that allows blood to leak into the GI lumen (area where food and fluid is processed for absorption or removal as waste). For example, a bleeding ulcer in the stomach can have the blood excreted in the person's fecal material.
- Rectal bleeding may be due to problems in the rectum itself or from many other problems that occur elsewhere in the GI tract. Perirectal bleeding is bleeding in an area adjacent to the rectum and may be due to abscesses or fistulas.
What Causes Bleeding From the Rectal Area?
There are many causes of rectal bleeding.
Common causes include
- hemorrhoids,
- anal fissure,
- diverticulosis,
- infection,
- inflammation (IBD or irritable bowel disease, Crohn's disease, colitis),
- blood vessel problems (angiodysplasia).
Other causes of rectal bleeding include
- polyps,
- tumors,
- trauma,
- an upper gastrointestinal source like stomach ulcers, and
- Meckel's diverticulum (rare).
Ischemia of the bowel occurs when blood flow to the bowel reduces or stops. For example, ischemic colitis usually occurs at the junction of the transverse and descending colon and can produce bright red or maroon blood.
Rectal Bleeding, Anorectal Disorders
Anorectal disorders are the most common causes of minor rectal bleeding.
Hemorrhoids: Hemorrhoids are swollen rectal veins in the anal and rectal area. They can cause burning, painful discomfort, and bleeding.
- External hemorrhoids are small swellings that are easy to see and quite painful. Anal itching is common.
- Internal and external hemorrhoids are usually painless. A person may note a rectal mass sensation with bowel movements.
- Symptoms from the swelling (thrombosis) of the hemorrhoids are brought on by hard stools and straining with bowel movements. Treatment of hemorrhoids focuses on relieving these symptoms with the use of stool bulking agents and softeners.
- In cases of thrombosed hemorrhoids, a clot forms within the swollen vein. This causes moderate to severe pain and requires minor surgery to remove them.
Anal fissure: This is a tear in the lining of the rectum caused by the passage of hard stools.
- An anal fissure can lead to mild rectal bleeding of bright red blood. Exposed nerves and vessels result in moderate to severe pain. Pain worsens with bowel movements then decreases in between bowel movements.
- In both hemorrhoids and anal fissures, symptoms generally improve with use of stool softeners and bulking agents, increasing fiber in the diet, pain control, and frequent warm water baths.
Diverticulosis: Diverticula are out-pouchings that project from the bowel wall. A low-fiber diet causes their development. When the diverticula becomes inflamed and infected, it is called diverticulitis.
- People with this condition are usually older than 40 years of age, and it generally increases with age.
- Stools are dark red or maroon. Pain is usually absent but, when present, typically occurs in the left lower part of the abdomen.
- Persistent bleeding, high fever, uncontrolled pain or other signs of serious infection may mean hospitalization is necessary. Fewer than 6% of patients with diverticulitis require surgery.
Infection: Bacterial dysentery is commonly the source of infectious, bloody diarrhea.
- Responsible organisms include Campylobacter jejuni, Salmonella, Shigella, Escherichia coli, and Clostridium difficile.
- Physical complaints include abdominal pain, fever, and bloody diarrhea.
- Medical professionals may administer antibiotics for treatment.
Inflammation: Inflammatory bowel disease (IBD) is a common cause of rectal bleeding in adults, typically younger than 50 years of age.
- Two common types of IBD include Crohn's disease and ulcerative colitis.
- Bleeding occurs in small to moderate amounts of bright red blood in the rectum, usually mixed in with stool and mucus. Associated symptoms include fever and cramping, stomach pain.
- Admission to the hospital is not required. However, bowel rest and steroid therapy are usually indicated for treatment.
Angiodysplasia: This is a vascular problem involving enlarged veins and capillaries in the wall of the right colon. These areas become fragile and can bleed.
- Episodes appear mainly in elderly people.
- Rectal bleeding is usually slow, chronic, and not obvious until massive bleeding occurs. People complain of weakness, fatigue, shortness of breath, and painless rectal bleeding.
Rectal Bleeding Tumors, Colon Polyps, and Other Causes
Polyps: Lumps of tissue or polyps bulge out from the lining of the colon. Bleeding occurs when large polyps develop, which can be hereditary. Usually harmless, some types can be precancerous.
Tumors: Both benign and malignant forms frequently appear in the colon and rectum. People older than 50 years of age are most affected. However, tumors also appear in younger people.
- Few people with tumor or polyps will have rectal bleeding. When bleeding does occur, it is usually slow, chronic, and minimal.
- If cancerous lesions are advanced, additional symptoms such as weight loss, a change in the caliber of stools, a sense of rectal fullness, or constipation may be experienced.
- Diagnosis requires evaluation with colonoscopy.
Trauma: Rectal bleeding from a traumatic cause is always a critical concern. Rectal damage from a gunshot wound or foreign body insertion can result in extensive infection or rapid and fatal blood loss. Prompt emergency evaluation is necessary.
Upper gastrointestinal source: A common source of rectal bleeding is bleeding from the upper gut, usually the stomach or duodenum. This can occur after someone has swallowed a foreign object that causes injury to the stomach lining, bleeding stomach ulcers, or Mallory-Weiss tears. (Mallory-Weiss tears are cuts or ruptures of vessels in the lining of the esophagus or stomach. They are usually due to continuing or forceful vomiting.)
- Long-term, chronic alcohol consumption can also cause ulcers, esophageal varices, and gastritis. All of these upper GI tract problems can bleed so briskly that people may note blood in the stool or in the rectum.
Meckel's diverticulum: A rare condition, where gastric lining appears in an inappropriate location of the gastrointestinal tract. As a result, the gastric acid secreted from this lining erodes tissue and ultimately causes hemorrhage. Although rare, it is the most common cause of gastrointestinal tract bleeding (GI bleeding) in children and young adults.
- Rectal bleeding in a Meckel's diverticulum is painless and appears bright red. Admission to the hospital is essential because surgery is often definitive treatment.
What Are the Signs and Symptoms of Rectal Bleeding?
- Rectal pain
- Bright red blood present in or on the stool
- Pain in the stomach, lower abdomen, rectum, or back
- Change in stool color to black, red, or maroon
- Stool test positive for occult blood loss (blood may present, but you cannot see it)
- Confusion
- Dizziness, lightheadedness
- Fainting, palpitations or rapid heartbeat
Rectal Bleeding in Children
Take rectal bleeding in small children seriously. Some children may require admission to the hospital and evaluation by a surgeon.
Intussusception: This condition occurs when the bowel folds in upon itself. It is the most common cause of intestinal obstruction and rectal bleeding in children up to 36 months. A majority of cases occur within the first year of life.
The three cardinal symptoms are:
- intermittent abdominal pains,
- vomiting, and
- rectal bleeding that looks like currant jelly.
However, these are not always present. Admission to the hospital is warranted because observation, further imaging tests, and surgery may be required.
Meckel's diverticulum: With this rare condition, gastric lining is incorporated into the GI tract but not in the stomach. Consequently, gastric acid secreted from this lining erodes tissue and may cause bleeding and ulcerations; it is the most common cause of GI bleeding in children and young adults.
Rectal Bleeding During Pregnancy
Hemorrhoids in the second and third trimesters of pregnancy are common. The cause is generally an increased pressure on the blood vessels in the pelvic area. Constipation and straining during bowel movements can also put pressure on the blood vessels. Straining during delivery can also exacerbate hemorrhoids.
If rectal bleeding occurs during pregnancy, even if a woman suspects the cause to be hemorrhoids, consult a physician.
When to Seek Medical Care for Rectal Bleeding
When rectal bleeding is present with one or more of the following symptoms, call a doctor:
- Stomach pain or swelling
- Nausea or vomiting
- Bleeding continues or worsens
- Recent weight loss
- Altered bowel habits
- Severe or prolonged diarrhea
- Pencil-sized stools, involuntary seepage of stools, or inability to have a bowel movement
If any of these signs and symptoms are present, one should visit the hospital's emergency department:
- Black or maroon stools
- Large volume blood loss
- Rectal pain or trauma
- Vomiting blood or other areas of the body bleeding or bruising
- Fever
- If the patient is on blood thinners
- Dizziness, weakness, passing out, or fainting spells
- Rapid or irregular heartbeat
- Difficulty breathing
What Procedures and Tests Diagnose Rectal Bleeding?
A physician will perform a physical examination. If necessary, diagnostic tests may be ordered.
Physical exam: The focus is on finding the source and extent of bleeding. Priority is to identify significant low blood volume and begin appropriate treatment. This is the most life-threatening situation. The physician will focus on three aspects:
- Vital signs: Low blood pressure and elevated heart rate will indicate significant loss of blood. An elevated temperature will suggest infection.
- Abdominal examination: The physician will search for abdominal distension, discomfort, or tenderness that may suggest a possible bleeding ulcer. A mass the doctor can feel is cause for concern about cancer.
- Anal and digital rectal examination: A medical professional will inspect the anus for possible external sources of bleeding such as trauma, foreign body, or hemorrhoids. A finger examination can assess tenderness, character of stool, and the presence of masses.
Diagnostic tests: Depending on the type and severity of bleeding, health care providers may perform special tests to aid in diagnosis.
- Blood tests: Health care professionals will take blood samples to assess the extent of blood loss, the clotting ability of blood, and the possibility of infection.
- Nasogastric tube: A medical professional may need to pass a flexible tube through the nose into the stomach to check for the presence of active bleeding. This may be uncomfortable, but can be a vital diagnostic test.
Scope examinations:
- Anoscopy: A plastic or metal scope (anoscope) placed into the anus allows for quick examination of the rectum.
- Flexible sigmoidoscopy: A flexible tube inserted into the rectum evaluates the rectum and lower end of the colon.
- Colonoscopy: A physician inserts a soft tube equipped with a light and camera into the rectum and pushes it into the colon. The medical professional can visualize the entire large colon. A colonoscopy can locate areas of bleeding, masses, or irregularities, and can be used to screen for colon cancer.
- Barium enema X-ray: This study uses liquid barium inserted into the rectum. An X-ray can highlight problem areas such as tumors or diverticula. However, it cannot distinguish sites of active bleeding.
- Nuclear medicine studies: A tagged red blood cell scan can pinpoint areas of slow bleeding.
- CT scan: This scan can help diagnose diverticulitis or tumors in the bowel.
- Angiography: A contrast dye study evaluates active areas of brisk bleeding.
What Is the Medical Treatment for Rectal Bleeding?
The treatment for rectal bleeding depends on the cause and source of the bleeding.
- Regardless of the source of bleeding, treatment of significant blood loss will begin by stabilizing the patient's condition.
- Initially, medical professionals will provide oxygen to the patient and monitor the heart. An IV will be started to administer fluids and for a possible blood transfusion.
- Further treatment options will depend on the suspected source of bleeding. A general surgeon, gastroenterologist, or ulcerative colitis specialist will likely become involved in the treatment plan.
- Admission to the hospital is required when a marked amount of blood loss has occurred, if bleeding has not stopped, or if vital signs have not become normal.
Home Remedies for Rectal Bleeding
If minimal rectal bleeding, such as blood-streaked toilet tissue, is the source of the problem, it may be due to hemorrhoids or a rectal fissure. Home therapy can be attempted. A physician should promptly evaluate and treat all other causes of rectal bleeding.
Self-care of rectal bleeding may include various rectal ointments and suppositories. People can buy these over-the-counter items without a prescription. If the person's symptoms do not improve within one week of treatment, or he or she is older than 40 years of age, a doctor should be seen for further evaluation.
Simple home care of rectal bleeding includes the following:
- Drink 8-10 glasses of water per day.
- Bathe or shower daily to cleanse the skin around the anus.
- Decrease straining with bowel movements.
- Increase fiber in the diet with supplements such as Metamucil, Benefiber, or foods such as prunes.
- Avoid sitting on the toilet too long.
- Apply ice packs to the affected area to decrease pain.
- Take a sitz bath. This is a warm water bath with water just deep enough to cover the hips and buttocks, and can help relieve some symptoms of itching, pain and discomfort of hemorrhoids.
- Avoid drinking alcohol, as that contributes to dehydration, which is one cause of constipation.
What Is the Follow-up for Rectal Bleeding?
Follow-up of treatment for rectal bleeding, especially if there are causes that resulted in heavy bleeding is important.
- See the doctor as scheduled.
- Take all prescribed medications as directed.
- Watch signs of continued rectal bleeding closely, as they will likely require re-evaluation.
What Is the Prognosis for Rectal Bleeding?
The majority of people with significant rectal bleeding are elderly. Members of this population commonly have many other medical problems. As a result, they tend to suffer increased rates of illness and death.
- In recent years, death from rectal bleeding has significantly decreased. This reduction is due to more efficient emergency departments, recent advances in procedures, and evolving surgical management.
- The majority of complications from rectal bleeding occur when large amounts of blood have been lost.
- The areas causing acute rectal bleeding may rebleed. This underscores the need for making a definitive diagnosis and in discovering the source of the bleeding so that the corrective actions may be made.
- Rectal bleeding with symptoms of weakness, dizziness, or fainting is associated with at least 1 liter (2 pints) of blood lost is a medical emergency. Seek medical care immediately. Sudden loss of 2 liters (4.2 pints) or more of blood can be dangerous, if not fatal.
Health Solutions From Our Sponsors
From 
Digestive Disorders Resources
Featured Centers
Health Solutions From Our Sponsors
American Cancer Society. “Colorectal Cancer.” 2019. <https://www.cancer.org/cancer/colon-rectal-cancer.html>.
Irizarry, L. “Acute Proctitis.” Medscape. Nov. 9, 2018. <https://emedicine.medscape.com/article/775952-overview>.
Penner, R.M., et al. "Patient information: Blood in the stool (rectal bleeding) in adults (Beyond the Basics)." UpToDate. February 2019.
<http://www.uptodate.com/contents/blood-in-the-stool-rectal-bleeding-in-adults-beyond-the-basics>.
United States. Centers for Disease Control and Prevention. “Basic Information About Colorectal Cancer.” Jan. 30, 2019. <https://www.cdc.gov/cancer/colorectal/basic_info/index.htm>.
United States. National Institutes of Health. National Institute of Diabetes and Digestive and Kidney Diseases. “Definition & Facts for Diverticular Disease.” <https://www.niddk.nih.gov/health-information/digestive-diseases/diverticulosis-diverticulitis/definition-facts>.
Vo, N., Thomas T.S., et al. "Intussusception in Children." UpToDate. March 22, 2019. <http://www.uptodate.com/contents/intussusception-in-children>.